The Hidden Predictors of Longevity: 3 Critical Metrics Your Annual Physical Is Missing
- Category: Health
- Published: Tuesday, 09 December 2025 12:46
- Tony Mathews
 (Submitted by By Tony Mathews, MD, MPH)
(Submitted by By Tony Mathews, MD, MPH)
In Scarsdale, we plan meticulously for the future. We manage our portfolios, our estates, and our children’s education with a long-term strategy. Yet, when it comes to the asset that underpins everything else—our physiology—many of us are flying blind.
Most high-performing individuals rely on an annual physical to gauge their health. If the standard labs come back “normal,” we assume we are safe.
However, as a physician practicing at the intersection of Endocrinology and Preventive Cardiology, I often see a disconnect between “normal” blood work and true longevity. Standard physicals are designed to detect active disease, not to map the silent trajectory of risk.
To manage your health more like an asset, you often need to look beyond the basic panel. Here are three silent metrics that rarely appear on a standard report but are critical for predicting your future health span.
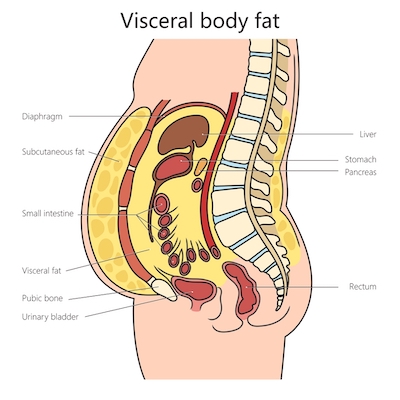
1. Visceral Adipose Tissue (VAT)
We are conditioned to focus on weight or BMI, but these are blunt instruments. Two people can weigh exactly the same yet have vastly different risk profiles based on where that mass is stored.
Visceral fat is the hidden fat stored deep inside the abdomen, wrapping around the liver and pancreas. Unlike subcutaneous fat (the kind you can pinch), visceral fat is metabolically active. It acts like a toxic organ, releasing inflammatory cytokines that drive insulin resistance and vascular damage.
You can have a “normal” BMI and still have dangerous levels of visceral fat—a pattern sometimes called “skinny fat” or metabolically obese normal weight. Advanced body composition analysis is the only way to track this metric accurately.
2. VO₂ Max: The Engine of Longevity
Often viewed as a metric for elite athletes, VO₂ max is actually one of the strongest predictors of all-cause mortality. It measures the maximum amount of oxygen your body can utilize during intense exercise.
Think of it as the horsepower of your cardiovascular system. A higher VO₂ max is associated with a significantly lower risk of heart disease, dementia, and certain cancers.
If you don’t know your number, you can’t manage it. Integrating clinical fitness testing into your medical plan moves exercise from a generic suggestion (“go to the gym”) to a precise prescription based on your current capacity.
3. Insulin Sensitivity, ApoB, and Lp(a)
A standard lipid panel gives you LDL, but often misses the nuance of particle number. Apolipoprotein B (ApoB) provides a more accurate count of the atherogenic particles driving plaque formation.
Similarly, a fasting glucose test only reveals your blood sugar at that moment, not how hard your pancreas worked to keep it there. Measuring fasting insulin and estimating insulin resistance (for example, with HOMA-IR) can uncover metabolic dysfunction years before prediabetes appears.
Finally, lipoprotein(a), or Lp(a), can reveal inherited cardiovascular risk that does not show up on a standard panel. Lp(a) is largely genetically determined and, when elevated, is associated with a higher risk of heart attack and stroke. Knowing your level helps your physician tailor the intensity of your risk-reducing strategies.
From Annual Checkups to a “Family Health Office” Mindset
The human body is an interconnected system. Hormones affect lipids; muscle mass affects insulin; inflammation affects the heart. Treating these in silos—or checking them only once a year—is a reactive strategy.
Some physicians use the term “Family Health Office” to describe a more integrated approach, where a medical team looks at cardiovascular, metabolic, and endocrine risks together over time. In this mindset, metrics like visceral fat, VO₂ max, insulin sensitivity, ApoB, and Lp(a) are not “extra tests,” but tools for understanding long-term risk.
You don’t need a new label to benefit from this approach. If you’ve never measured these metrics, ask your physician if these evaluations are appropriate for you. The goal is to catch subtle patterns early, when targeted treatment and lifestyle changes can still meaningfully shape your future health span.
This article is for informational purposes only and is not a substitute for personal medical advice. Always discuss specific testing or treatment decisions with your own physician. Dr. Tony Mathews, MD, MPH, is dual fellowship–trained and quadruple board-certified in Internal Medicine, Endocrinology, Obesity Medicine, and Clinical Lipidology, with over 12 years of clinical experience. He has spent the past three years caring for patients in Bronxville, Scarsdale, and the surrounding Westchester communities.
Dr. Tony Mathews, MD, MPH, is dual fellowship–trained and quadruple board-certified in Internal Medicine, Endocrinology, Obesity Medicine, and Clinical Lipidology, with over 12 years of clinical experience. He has spent the past three years caring for patients in Bronxville, Scarsdale, and the surrounding Westchester communities.
He practices at Sequoia Medical 360 (116 Kraft Ave, Suite 4, Bronxville, NY, 914-292-0300), a physician-led practice that uses a “Family Health Office” model to organize long-term cardiovascular, metabolic, and endocrine care. Sequoia Medical 360 participates with Medicare and most private insurance plans.