The Hidden Predictors of Longevity: 3 Critical Metrics Your Annual Physical Is Missing
- Details
- Written by: Tony Mathews
- Category: Health
 (Submitted by By Tony Mathews, MD, MPH)
(Submitted by By Tony Mathews, MD, MPH)
In Scarsdale, we plan meticulously for the future. We manage our portfolios, our estates, and our children’s education with a long-term strategy. Yet, when it comes to the asset that underpins everything else—our physiology—many of us are flying blind.
Most high-performing individuals rely on an annual physical to gauge their health. If the standard labs come back “normal,” we assume we are safe.
However, as a physician practicing at the intersection of Endocrinology and Preventive Cardiology, I often see a disconnect between “normal” blood work and true longevity. Standard physicals are designed to detect active disease, not to map the silent trajectory of risk.
To manage your health more like an asset, you often need to look beyond the basic panel. Here are three silent metrics that rarely appear on a standard report but are critical for predicting your future health span.
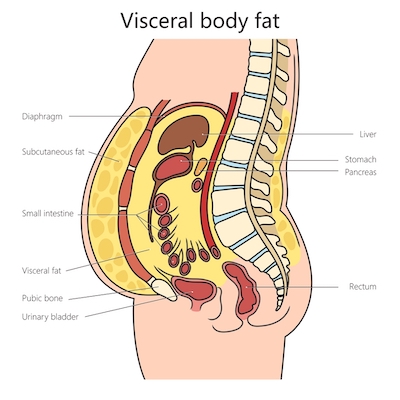
1. Visceral Adipose Tissue (VAT)
We are conditioned to focus on weight or BMI, but these are blunt instruments. Two people can weigh exactly the same yet have vastly different risk profiles based on where that mass is stored.
Visceral fat is the hidden fat stored deep inside the abdomen, wrapping around the liver and pancreas. Unlike subcutaneous fat (the kind you can pinch), visceral fat is metabolically active. It acts like a toxic organ, releasing inflammatory cytokines that drive insulin resistance and vascular damage.
You can have a “normal” BMI and still have dangerous levels of visceral fat—a pattern sometimes called “skinny fat” or metabolically obese normal weight. Advanced body composition analysis is the only way to track this metric accurately.
2. VO₂ Max: The Engine of Longevity
Often viewed as a metric for elite athletes, VO₂ max is actually one of the strongest predictors of all-cause mortality. It measures the maximum amount of oxygen your body can utilize during intense exercise.
Think of it as the horsepower of your cardiovascular system. A higher VO₂ max is associated with a significantly lower risk of heart disease, dementia, and certain cancers.
If you don’t know your number, you can’t manage it. Integrating clinical fitness testing into your medical plan moves exercise from a generic suggestion (“go to the gym”) to a precise prescription based on your current capacity.
3. Insulin Sensitivity, ApoB, and Lp(a)
A standard lipid panel gives you LDL, but often misses the nuance of particle number. Apolipoprotein B (ApoB) provides a more accurate count of the atherogenic particles driving plaque formation.
Similarly, a fasting glucose test only reveals your blood sugar at that moment, not how hard your pancreas worked to keep it there. Measuring fasting insulin and estimating insulin resistance (for example, with HOMA-IR) can uncover metabolic dysfunction years before prediabetes appears.
Finally, lipoprotein(a), or Lp(a), can reveal inherited cardiovascular risk that does not show up on a standard panel. Lp(a) is largely genetically determined and, when elevated, is associated with a higher risk of heart attack and stroke. Knowing your level helps your physician tailor the intensity of your risk-reducing strategies.
From Annual Checkups to a “Family Health Office” Mindset
The human body is an interconnected system. Hormones affect lipids; muscle mass affects insulin; inflammation affects the heart. Treating these in silos—or checking them only once a year—is a reactive strategy.
Some physicians use the term “Family Health Office” to describe a more integrated approach, where a medical team looks at cardiovascular, metabolic, and endocrine risks together over time. In this mindset, metrics like visceral fat, VO₂ max, insulin sensitivity, ApoB, and Lp(a) are not “extra tests,” but tools for understanding long-term risk.
You don’t need a new label to benefit from this approach. If you’ve never measured these metrics, ask your physician if these evaluations are appropriate for you. The goal is to catch subtle patterns early, when targeted treatment and lifestyle changes can still meaningfully shape your future health span.
This article is for informational purposes only and is not a substitute for personal medical advice. Always discuss specific testing or treatment decisions with your own physician. Dr. Tony Mathews, MD, MPH, is dual fellowship–trained and quadruple board-certified in Internal Medicine, Endocrinology, Obesity Medicine, and Clinical Lipidology, with over 12 years of clinical experience. He has spent the past three years caring for patients in Bronxville, Scarsdale, and the surrounding Westchester communities.
Dr. Tony Mathews, MD, MPH, is dual fellowship–trained and quadruple board-certified in Internal Medicine, Endocrinology, Obesity Medicine, and Clinical Lipidology, with over 12 years of clinical experience. He has spent the past three years caring for patients in Bronxville, Scarsdale, and the surrounding Westchester communities.
He practices at Sequoia Medical 360 (116 Kraft Ave, Suite 4, Bronxville, NY, 914-292-0300), a physician-led practice that uses a “Family Health Office” model to organize long-term cardiovascular, metabolic, and endocrine care. Sequoia Medical 360 participates with Medicare and most private insurance plans.
Pregnancy & Diabetes: Know the Risk
- Details
- Written by: Joanne Wallenstein
- Category: Health
 Submitted by Gayotri Goswami, MD, FACE, Endocrinology at White Plains Hospital
Submitted by Gayotri Goswami, MD, FACE, Endocrinology at White Plains Hospital
Gestational diabetes mellitus (GDM) can be an unexpected development during pregnancy — but with awareness, timely testing, and a healthy lifestyle, you can help prevent it or at least manage it effectively.
Similar to type 2 diabetes, GDM can in many instances go away once the baby is delivered. Nevertheless, The Centers for Disease Control & Prevention estimates that every year, 5% to 9% of pregnancies in the U.S. are affected by GDM.
Although researchers have yet to pinpoint why some women develop gestational diabetes and others do not, they have identified some risk factors for developing the disease, which include:
• Having had GDM during a previous pregnancy
• Having birthed a baby weighing over 9 pounds
• Being overweight
• Being over 25 years old
• Having a family history of type 2 diabetes
• Being a person of color
During pregnancy, hormone levels shift, and while they usually help keep blood sugar stable, sometimes they don’t—making it harder for your body to process sugar efficiently. Gestational diabetes can also raise your risk of high blood pressure during pregnancy.
GDM can also lead to a bigger baby, early delivery with breathing issues, low blood sugar at birth, or a higher risk of type 2 diabetes later on.
Overcoming GDM
GDM rarely comes without warning. Most pregnant women are screened for high glucose levels between 24 and 28 weeks—or sooner if earlier tests or risk factors suggest the need.
Once your baby’s here, your blood sugar should bounce back. Follow up with your doctor 6 to 12 weeks later—and every few years—to keep it that way. A Certified Diabetes Care and Education Specialist (CDCES) can help tailor a plan that works for you.
Eating healthier is a smart move for everyone, no matter where you are on your journey. Try following the MyPlate model (myplate.gov), filling half your plate with fruits and veggies. And aim for about 30 minutes of activity a day—even a brisk walk counts.
With proper precautions and education, GDM does not have to be a frightening prospect. Discuss your background and risk factors with your provider during one of your regular prenatal visits; they will refer you to an endocrinologist if necessary.
Dr. Gayotri Goswami is an endocrinologist with White Plains Hospital Physician Associates. To make an appointment, call 914-849-7400.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.
Letter to the Editor: Missed Water Bill and Late Charges
- Details
- Written by: Joanne Wallenstein
- Category: Health
 Here is a letter from a Scarsdale resident concerning their water bill. He reports that he did not receive his bill in August and was assessed late fees and a penalty on the November bill. Did you have a similar experience? Please comment below:
Here is a letter from a Scarsdale resident concerning their water bill. He reports that he did not receive his bill in August and was assessed late fees and a penalty on the November bill. Did you have a similar experience? Please comment below:
(From Mr. Ruder)
We just received our 11/1/25 water bill from Scarsdale. It included the fees for May-July and August-October as well as a penalty for non-payment of the first piece. I called the water department and told them that in 28 years here in Scarsdale, we had never missed a payment deadline and that I did not receive the May-July invoice....so I did not pay it.
They said that they were aware of a number of residents who did not receive their May-July bill. They will let me know if they will waive the penalty as they consider their response to this situation. I can only hope that they are reasonable and fair in their decision-making here.
This is so similar to the "lost" school tax bills from a couple of years ago. It seems that something remains broken in the Scarsdale system for getting these important documents out to residents.
Brian Ruder
We asked Scarsdale Village Manager Alexandra Marshall for a comment and here is what she shared: "The Water Department staff forwarded me your question. At this time, we have been contacted by 76 water account customers who have indicated they did not receive their August water bill. As calls come in, water department staff continue to work with costumers to resolve their billing concerns. Recognizing concerns from the public about reliability of postal service, the Village continues to put out additional electronic reminders about important upcoming bill/collection deadlines. Staff have also been exploring tools to make payment of bills easier for our residents."
Living Well with IBD
- Details
- Written by: Joanne Wallenstein
- Category: Health
 (Submitted by Dr. Amneet Hans, Gastroenterology)
(Submitted by Dr. Amneet Hans, Gastroenterology)
Sudden abdominal pain, urgent trips to the restroom, and other symptoms including bleeding and weight loss are an everyday reality for many people living with inflammatory bowel disease (IBD) — a chronic autoimmune condition in which the immune system attacks healthy tissue in the digestive tract.
The two main types of IBD – Crohn’s disease and ulcerative colitis – affect an estimated 2.4 to 3.1 million Americans. Crohn’s disease can affect different segments of the digestive tract, from the mouth to the anus, and symptoms may be subtle at first, starting with nutritional deficiency like low iron levels and vague abdominal pain. Ulcerative colitis only affects the colon but is characterized by the more urgent gastrointestinal symptoms.
While there is no cure for IBD, treatments have advanced significantly over the past few decades and now include a variety of options such as topical, oral, injectable, or intravenous medications.
The White Plains Hospital Approach
White Plains Hospital’s Inflammatory Bowel Disease Program, which brings together comprehensive diagnostic and treatment services, is overseen by its Associate Director, board-certified gastroenterologist Dr. Amneet Hans. “It’s best to treat IBD early, to prevent long-term complications, which include increased risk of colon cancer,” she says.
Cases are steadily rising, partly because of improved diagnosis, but doctors also theorize that stress and a Western diet, heavy with processed foods, could play a role. IBD symptoms can also mimic other conditions, such as food poisoning or lactose intolerance. But if problems like cramping, diarrhea, or blood in the stool persist for several weeks, it is time to call your doctor.
Program participants meet with Dr. Hans or one of her colleagues every few weeks until symptoms are under control. Once a patient is in remission, follow-up visits are typically scheduled every three to six months. These visits may include blood tests, stool testing (such as fecal calprotectin), or a colonoscopy to assess for endoscopic remission — evidence that the lining of the colon has healed. For some patients, IBD medications may not be the best option or there are other complications that may not respond to medical therapy. In these cases, patients may be referred to the program’s colorectal surgery specialists, Dr. Kimberly Yee, Dr. June Hsu, or Dr. Yadin Bornstein, to discuss how surgery may help relieve their symptoms. “Shared decision-making is an important component of IBD care,” explains Dr. Hans. “I discuss different treatment options with each patient, help them understand their diagnosis, and achieve and stay in remission. Building long-term relationships and seeing patients regain their quality of life is very rewarding.”
For some patients, IBD medications may not be the best option or there are other complications that may not respond to medical therapy. In these cases, patients may be referred to the program’s colorectal surgery specialists, Dr. Kimberly Yee, Dr. June Hsu, or Dr. Yadin Bornstein, to discuss how surgery may help relieve their symptoms. “Shared decision-making is an important component of IBD care,” explains Dr. Hans. “I discuss different treatment options with each patient, help them understand their diagnosis, and achieve and stay in remission. Building long-term relationships and seeing patients regain their quality of life is very rewarding.”
Dr. Amneet Hans is Associate Director of the Inflammatory Bowel Disease (IBD) Program at White Plains Hospital. Board-certified in Gastroenterology and Internal Medicine, Dr. Hans practices in White Plains and specializes in the medical and endoscopic management of IBD, including Crohn’s disease and ulcerative colitis. To make an appointment, call (914) 948-1000.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.
Move with Purpose: How Smart Exercise Improves Longevity, Metabolic Health, and Strength
- Details
- Written by: Joanne Wallenstein
- Category: Health
 Submitted By Tony Mathews, MD, MPH
Submitted By Tony Mathews, MD, MPH
We all know exercise is essential for health. But for those striving not just to live longer — but live better — movement becomes more than a daily habit. It’s medicine.
At Sequoia Medical 360, we combine precision diagnostics with performance science to help patients move with intention, not guesswork. In partnership with Sensei Leo Lopes and Total Form Fitness Scarsdale, we design evidence-based programs that target metabolic health, strength, and longevity — from Zone 2 endurance to high-intensity interval bursts and functional resistance training.
1. Train Your Mitochondria: The Power of Zone 2
Zone 2 training is moderate exercise that keeps your heart rate in the 60–70% range of your maximum — brisk enough to raise your breathing, but still conversational. Think of it as a gentle, sustained challenge that trains your mitochondria, the “power plants” of your cells.
Regular Zone 2 work improves fat metabolism, insulin sensitivity, and cardiovascular efficiency — three pillars of longevity. Just 30–45 minutes, three to four times a week, can profoundly shift your metabolic health.
2. Challenge Your Limits: The Longevity Boost of HIIT
High-Intensity Interval Training (HIIT) takes things up a notch — short bursts of vigorous effort alternated with recovery periods. This form of training can increase VO₂ max, a key measure of your body’s oxygen efficiency and one of the strongest predictors of lifespan.
Even 10–20 minutes of structured HIIT twice a week can enhance endurance, improve blood sugar control, and strengthen heart resilience.
3. Build Strength, Prevent Sarcopenia
After 30, we begin losing about 1% of muscle mass each year — a process called sarcopenia. The antidote is simple but powerful: resistance training at least twice a week.
You don’t need heavy barbells; bodyweight, resistance bands, or light dumbbells can all help build lean muscle. The goal is to preserve independence, mobility, and metabolic strength for life.
4. The Japanese Walking Method: Simple, Sustainable Fitness
Recent research from Japan highlights a remarkably effective routine: three minutes of brisk walking followed by three minutes of leisurely strolling, repeated for 30 minutes.
This rhythm alternates intensity, boosts endurance, and keeps joints happy — ideal for beginners or those easing back into fitness. Walking remains one of the most powerful and underappreciated forms of medicine.
5. Can You Exercise Too Much?
Absolutely — when exercise becomes excessive, it can raise cortisol, suppress immunity, and cause burnout or injury.
The key is balance and purpose. Movement should energize you, not deplete you. Rest, recovery, and mindful listening to your body are as essential as your workouts.
You’re not just training for today — you’re conditioning your body for decades of vitality.
6. Where Medicine Meets Movement
At Sequoia Medical 360, we measure what matters — from VO₂ max and metabolic markers to hormonal and bone health — and collaborate with our partners at Total Form Fitness to turn data into action. Together, we help you train intelligently, age powerfully, and move with purpose.
Take the First Step
Ready to understand your body and optimize your fitness for life?
Schedule your comprehensive medical and performance assessment today with Dr. Tony Mathews and Sensei Leo Lopes — your partners in proactive health and longevity.
Dr. Tony Mathews is a Dual Fellowship-Trained, Quadruple Board-Certified Endocrinologist and Longevity Medicine Specialist with over 12 years of experience, who has spent the past 3 years serving our local community.
Sequoia Medical 360 is a Concierge Medical Practice based out of Bronxville and serves the Westchester community. We accept Medicare and Most Private Insurances.
Sequoia Medical 360 – 116 Kraft Ave, Suite 4, Bronxville, NY
Total Form Fitness – Scarsdale, NY
(914) 292-0300 | www.SQMed360.com